 |
 |
AbstractBackground and ObjectivesFor plunging ranula, excision of the sublingual gland has been the major treatment option, with sclerotherapy being widely used as minimal invasive treatment. We compared the outcomes of these two methods as an initial treatment for ranula and investigated the outcomes of salvage procedure in recurred patients.
Subjects and MethodPatients were classified into the excision group (n=35) and the sclerotherapy group (n=39) according to the type of their initial treatment. The outcomes of the initial and salvage treatment were determined as recurrence or non-recurrence at 3 months after treatment, and statistically compared between the excision and the sclerotherapy groups.
ResultsRecurrence in the sclerothearpy group (n=20, 51.3%) showed a significantly higher rate (p<0.001) than in the excision group (n=3, 8.6%). Recurring patients who received treatment different from the initial treatment (n=7) were cured, while those who had same procedure as the initial treatment (n=11) showed recurrence of 72.7% (n=8). There was no procedure related complication among the patients.
IntroductionThe ranula is a retention cyst made of extravasated saliva from a damaged salivary duct or gland [1,2]. Ranula could be presented as intraoral or submandibular mass. An intraoral ranula is confined to the floor of the mouth and a plunging ranula is herniated cyst located below the mylohyoid muscle and present as a lump in the upper part of the neck [3].
Various treatment methods have been practiced based on different concepts of pathogenesis. Simple excision of ranula, cyst extirpation, excision of the sublingual gland, and sclerotherapy of ranula sac have been popular procedures for treatment of ranula [4,5]. Pathological studies reported that most ranulas are pseudocysts without epithelial lining arisen from sublingual gland [4,6]. Therefore, simple excision and extirpation of ranula have been avoided which targeted only ranula sac, not sublingual gland. Excision of the sublingual gland is recently considered to be a reasonable treatment [7,8]. However, excision of sublingual gland demonstrated several disadvantages such as insufficient removal of sublingual gland, necessity of general anesthesia and the risk of damage to the adjacent structures including the submandibular gland duct and lingual nerve [9]. Therefore, nonsurgical therapies with less associated morbidity have been required for the treatment of ranula. Sclerosing agents including OK-432 (picibanil), bleomycin, and ethanol have been introduced to be highly effective and minimal invasive in the treatment of ranula [2,10-12]. They evoke inflammatory reaction and increased endothelial permeability that lead to shrinkage of the cystic space.
There has been no consensus about the definitive management of plunging ranula because of a lot of variation between previous studies. Previous studies enrolled the subjects with heterogenous types of ranula and they did not focus on plunging ranula or intraoral ranula which could affect to treatment methods and outcomes [13-15]. Furthermore, they had practiced inconsistent procedures such as sublingual gland excision, ranula excision or extirpation. In addition, they did not report about clinical course and salvage treatment after failure of initial treatment. Therefore, the aim of study was to evaluate the treatment outcomes of sublingual gland excision and ethanol sclerotherapy for plunging ranula and investigated the salvage treatment and outcomes of recurred ranula after initial treatment.
Subjects and MethodsPatientsThis study was approved by Institutional Review Board (2020-09-016) of authorsŌĆÖ hospital. Total 223 patients had visited our clinic for the management of sublingual gland ranula from 2002 to 2019. Patients who had intraoral ranula (n=119), repeated aspiration of ranula (n=17), and observation without treatment (n=13) were excluded (Fig. 1). Finally, 74 patients were analyzed who received excision of sublingual gland (excision group, n=35) and sclerotherapy of ranula (sclerotherapy group, n=39). All patients had been observed more than 3 months after initial procedure and we performed additional procedures for patients who revealed recurrent plunging ranula. Recurrent patients were also observed until 3 months after salvage surgery and treatment outcomes were investigated at the last follow-up.
Preoperative evaluation and outcome measurementThe patients received endoscopic assessment, contrast enhanced CT and ultrasound guided aspiration of ranula sac for identification of saliva content. After the preoperative evaluation, we counselled the patients about treatment methods, and then patients chose the excision of sublingual gland or ethanol sclerotherapy. We explained advantages and disadvantages of two treatment methods based on previous studies and our experiences. In general, patients who wanted to have lower recurrence rate choose the excision of sublingual gland and patients who were reluctant to have surgery under general anesthesia choose the sclerotherapy. The patients had visited every month until 3 months after procedure. Patients had been examined by history taking and physical examination at each visit. If recurrence of plunging ranula was suspected by physical examination and subjective symptoms, we performed ultrasonography or CT. Treatment outcomes were determined as recurrence or non-recurrence at 3 months after procedure.
Sublingual gland excisionExcision of sublingual gland was performed under general anesthesia. Mouth floor incision was made along the shadow of sublingual gland and sublingual gland was totally removed while preserve lingual nerve and WhartonŌĆÖs duct. After the excision of sublingual gland, we extirpated ranula sac with metal suction tip intraorally.
Ethanol sclerotherapySclerotherapy was performed under local anesthesia by subcutaneous infiltration of 2% lidocaine, and we confirmed accurate needle location in the ranula sac during whole procedure by ultrasound guidance. A 18-gauge angiocatheter was connected with three-way stop cock and ranula sac was aspirated using 20 cc syringe. The syringe containing aspirated saliva was discarded, leaving the angiocatheter left in the ranula sac. Other syringe containing 2% lidocaine was connected to the three-way stop cock and we injected 2% lidocaine of 3 mL into the sac and waited 10 minutes before ethanol injection to reduce the pain and burning sensation. Lidocaine was aspirated and 98% ethanol of 3 mL was injected. The needle was removed and we educated the patients to press directly over injection site for 5 minutes.
Statistical analysisBaseline characteristics including age, sex and treatment outcome were compared between the excision group and sclerotherapy group. The Mann-Whitney test was used to compare continuous variables, and categorical variables were analyzed with FisherŌĆÖs exact test. p-value<0.05 was considered as statistically significant. Statistical analyses were performed using SPSS for Windows ver. 20.0 (IBM Corp., Armonk, NY, USA).
ResultsBaseline characteristics of the enrolled patientsMean age was 28.8┬▒13.1 years in the excision group and 28.3┬▒11.3 years in the sclerotherapy group, and it did not show statistical difference (p=0.737). The excision group consisted of 26 males and 9 females and the sclerotherapy group consisted of 25 males and 14 females. Distribution of sex was not significantly different (p=0.452) between the two groups (Table 1). In the sclerotherapy group, there was no complications like skin necrosis or infection, and pain was tolerable with oral acetaminophen in all patients.
Comparison of outcomes between the excision group and sclerotherapy group as an initial treatmentIn excision group, 3 (8.6%) of 35 patients had recurrence and 20 (51.3%) of 39 patients had recurrence in sclerotherapy group. Recurrence rate was significantly higher in sclerotherapy group (p<0.001).
Treatment after recurrence of initial treatmentWhen recurrence of ranula, we decided salvage procedure based on patientsŌĆÖ counselling. Among 3 recurred patients of the excision group, 2 patients had re-excision of remnant sublingual gland and 1 patient had sclerotherapy. After salvage treatment, 2 patients (1 excision and 1 sclerotherapy) were cured, and 1 patient who had re-excision was recurred and he was cured after sclerotherapy (Table 1).
Among 20 recurred patients of the sclerotherapy group, 2 (10.0%) had sublingual gland excision, 9 (45.0%) had resclerotherapy, and 9 (45.0%) had observation without treatment.
After salvage treatment, patients with sublingual gland excision (n=2) had no recurrence, but 7 of 9 (77.7%) patients who had re-sclerotherapy showed recurrent ranula again. Among those recurred patients (n=7), 4 patients were cured by excision of sublingual gland, 1 patient were cured by re-sclerotherapy (n=1), and 2 patients had regular observation without further treatment. There was no treatment related complication with initial and salvage treatment.
Notably, in the recurred cases, patients who had a different procedure than initial surgery (n=7) showed no recurrence. Especially in the sclerotherapy group, excision of sublingual gland was effective even in the patients who had recurrence after multiple sclerotherapy.
Otherwise, patients who underwent same procedure as the first procedure (n=11) recurred in 8 patients (72.7%).
DiscussionWe investigated the outcomes of excision of sublingual gland and ethanol sclerotherapy for plunging ranula as an initial and salvage treatment. Sublingual gland excision (recurrence rate of 8.6%) was identified as more effective treatment than sclerotherapy (recurrence rate of 51.3%), and two treatment methods might have complementary effect in recurred cases in our study.
Plunging ranula has unique clinical presentations in comparison with other types of ranula, which may appear as a submandibular mass without visible intraoral involvement [3]. In addition, plunging ranula and intraoral ranula showed different clinical courses and they required different approach for diagnosis and treatment [6,8,13,15]. However, many previous studies did not classify the subtype of ranula [13,15-17]. Therefore, it has been necessary to perform a large-scaled study confined to plunging ranula, and we focused on patients with plunging ranula to have homogeneous enrollment of subjects and obtain reliable results.
In addition, many previous studies have performed quite variable treatment methods including needle aspiration, surgical excision of the cyst, sublingual gland excision, marsupialization, and sclerotherapy [4,5,18,19]. Parekh, et al. [7] reported the outcomes of 139 plunging ranula that 70% of incision and drainage, 53% of marsupialization, 85% of excision of the cyst, 3.8% of cyst and sublingual gland excision together, and 0% of intraoral excision of the sublingual gland with drainage of cyst showed recurrence. Sigismund, et al. [20] reported that 13.6% of marsupialization, 3.6% of complete sublingual gland excision, and 36.4% of ranula excision alone were recurred after treatment. Crysdale, et al. [21] demonstrated that the incidence of recurrence was 100% after incision and drainage of ranula, 61% after simple marsupialization, and 0% after sublingual gland excision. Yang and Hong [22] demonstrated successful treatment in all 23 patients by the sublingual gland with evacuation of cyst.
As mentioned above, different types of surgery demonstrated quite variable treatment outcomes and sublingual gland excision has been accepted as the most effective treatment method [2,6,8]. In the excision group (n=35), we have consistently performed sublingual gland excision with ranula extirpation which showed recurrence rate of 9.6% as an initial treatment. Our study demonstrated relatively high recurrence rate in the excision group in comparison with previous studies. It caused by insufficient infection control before treatment and remained sublingual gland at posterior and deep mouth floor area.
Surgical excision of sublingual gland was the first choice of treatment, but many patients were reluctant to the invasive procedure under general anesthesia. Furthermore, insufficient surgery, recurrence, and the risk of damage to the adjacent structures including the submandibular gland duct and lingual nerve have been reported when performing sublingual gland excision [9]. Therefore, nonsurgical therapies with less associated morbidity have been also required for the treatment of ranula. OK-432 (picibanil), a sclerosing agent, has been widely used in previous studies which is highly effective and to have minimal side effects for the treatment of cystic lymphangioma and plunging ranula [2,10,23]. The mechanism of sclerotic agent is that it immediately evokes the infiltration of the inflammatory cells into the cystic spaces and extensive production of cytokines, including interleukin-6 and tumor-necrotic factor [24].
Fukase, et al. [24] reports 100% resolution of 11 cases of plunging ranula after multiple injections, but the success rate after the first injection was only 45.5%. Rho, et al. [14] found the success rate for treating plunging ranulas in their series was only 33.3% after one injection of OK-432. To the best of our knowledge, previous studies about sclerotherapy with OK-432 for plunging ranula were usually case series and not comparative study with other treatment methods and they did not describe the clinical course after failure of initial treatment. In addition, OK-432 has been hard to access in the South Korea and other countries including United States. In South Korea, physician should request drug before several weeks ago to Korea Orphan & Essential Drug Center.
Therefore, there has been several trials of ethanol injection for ranula [25,26], and we have also practiced ethanol sclerotherapy in this study and compared the outcomes between surgery and sclerotherapy. Previous retrospective study of 20 patients who had ethanol injection demonstrated that 9 patients (45%) demonstrated complete disappearance of the ranula and 11 (55%) showed partial response which was comparable to OK-432 sclerotherapy [26]. In our study, we performed the ethanol injection in the sclerotherapy group (n=39), and they have a recurrence rate of 51.3% as an initial treatment.
After initial treatment, 23 (31.1%) patients were recurred in the excision (n=3) and the sclerotherapy group (n=20). Interestingly, patients who recurred after initial treatment were all cured by salvage treatment different from initial treatment (n=7). Otherwise, patients who underwent same procedure with initial procedure (n=11) recurred in 8 patients (72.7%). Two treatment methods used in this study are based on different mechanism that the excision of sublingual gland is removal of the causative salivary gland and sclerotherapy targets leaked cyst with adjacent salivary gland. We assume that these two different treatment methods have complementary effect to each other in recurred patients. We found this complementary effect in 6 cases in the sclerotherapy group and only 1 case in the excision group. Therefore, we are careful to conclude because of the small number of recurred patients especially in the excision group, but two surgeries may have complementary effects to each other. After the failure of sclerotherapy, the excision of sublingual gland should be considered as a salvage treatment.
This study presented the comparison between the excision of sublingual gland and the sclerotherapy for the patients with plunging ranula and management of recurrence. We have limitations that it is difficult to perform the statistical analysis of management of recurrence because of small number of recurred cases especially in the excision group. In addition, this study was retrospective with non-randomized patient enrollment which could cause selection bias.
In conclusion, excision of sublingual gland is more effective treatment for plunging ranula than ethanol sclerotherapy as an initial treatment. In recurred cases after ethanol sclerotherapy, sublingual gland excision was also effective. We might consider the salvage treatment method other than the initial treatment to manage the recurred cases.
NotesAuthor Contribution Conceptualization: Nayeon Choi. Data curation: all authors. Formal analysis: Hyun Jung Kim, Nayeon Choi. Methodology: all authors. Project administration: Nayeon Choi. Visualization: Nayeon Choi. WritingŌĆöoriginal draft: all authors. WritingŌĆöreview & editing: all authors. Fig.┬Ā1.The patient with sublingual gland ranula (n=223) and enrollment and clinical courses of patients with plunging ranula treated with excision of sublingual gland (n=35) and ethanol sclerotherapy (n=39). 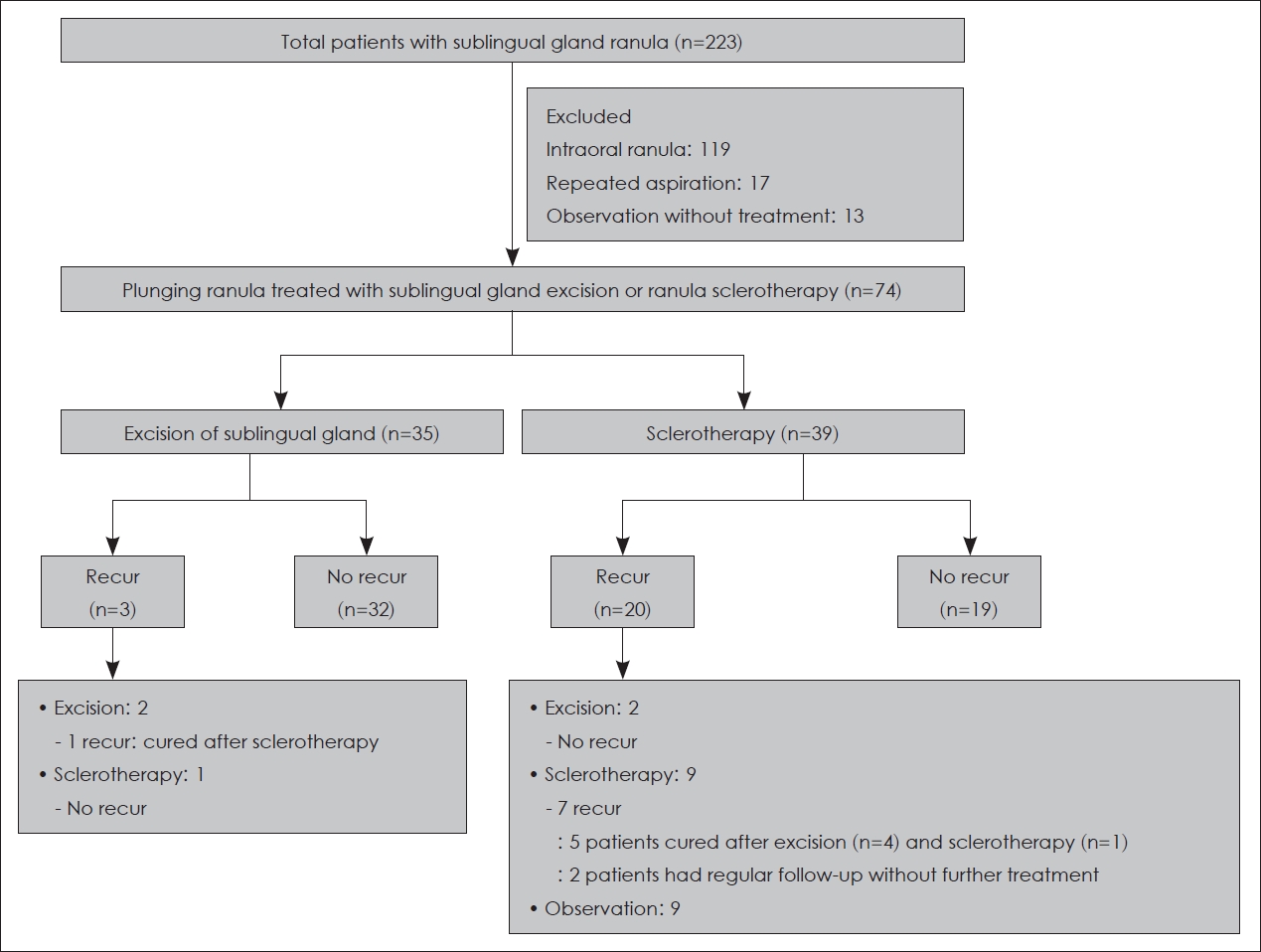
Table┬Ā1.Baseline characteristics and treatment outcomes of the sublingual gland excision group and the ranula sclerotherapy group (n=74) REFERENCES2. Baurmash HD. Marsupialization for treatment of oral ranula: A second look at the procedure. J Oral Maxillofac Surg 1992;50(12):1274-9.
3. McGurk M, Eyeson J, Thomas B, Harrison JD. Conservative treatment of oral ranula by excision with minimal excision of the sublingual gland: Histological support for a traumatic etiology. J Oral Maxillofac Surg 2008;66(10):2050-7.
4. Davison MJ, Morton RP, McIvor NP. Plunging ranula: Clinical observations. Head Neck 1998;20(1):63-8.
5. Zhi K, Gao L, Ren W. What is new in management of pediatric ranula? Curr Opin Otolaryngol Head Neck Surg 2014;22(6):525-9.
6. Yoshimura Y, Obara S, Kondoh T, Naitoh S. A comparison of three methods used for treatment of ranula. J Oral Maxillofac Surg 1995;53(3):280-2, discussion 283.
7. Parekh D, Stewart M, Joseph C, Lawson HH. Plunging ranula: A report of three cases and review of the literature. Br J Surg 1987;74(4):307-9.
8. Haberal I, G├Č├¦men H, Samim E. Surgical management of pediatric ranula. Int J Pediatr Otorhinolaryngol 2004;68(2):161-3.
9. Zhao YF, Jia J, Jia Y. Complications associated with surgical management of ranulas. J Oral Maxillofac Surg 2005;63(1):51-4.
10. Ikarashi T, Inamura K, Kimura Y. Cystic lymphangioma and plunging ranula treated by OK-432 therapy: A report of two cases. Acta Otolaryngol Suppl 1994;511:196-9.
11. Kim KH, Sung MW, Roh JL, Han MH. Sclerotherapy for congenital lesions in the head and neck. Otolaryngol Head Neck Surg 2004;131(3):307-16.
12. Kolker MT, Batti JS, Schoem SR. The ex utero intrapartum treatment procedure for congenital ranula in a JehovahŌĆÖs Witness. Otolaryngol Head Neck Surg 2004;130(4):508-10.
13. Than JK, Rosenberg TL, Anand G, Sitton M. The importance of sublingual gland removal in treatment of ranulas: A large retrospective study. Am J Otolaryngol 2020;41(3):102418.
14. Rho MH, Kim DW, Kwon JS, Lee SW, Sung YS, Song YK, et al. OK-432 sclerotherapy of plunging ranula in 21 patients: It can be a substitute for surgery. AJNR Am J Neuroradiol 2006;27(5):1090-5.
15. Zhao YF, Jia Y, Chen XM, Zhang WF. Clinical review of 580 ranulas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98(3):281-7.
16. Kokong D, Iduh A, Chukwu I, Mugu J, Nuhu S, Augustine S. Ranula: Current concept of pathophysiologic basis and surgical management options. World J Surg 2017;41(6):1476-81.
17. Roh JL. Primary treatment of ranula with intracystic injection of OK-432. Laryngoscope 2006;116(2):169-72.
18. Ichimura K, Ohta Y, Tayama N. Surgical management of the plunging ranula: A review of seven cases. J Laryngol Otol 1996;110(6):554-6.
19. Chidzonga MM, Mahomva L. Ranula: Experience with 83 cases in Zimbabwe. J Oral Maxillofac Surg 2007;65(1):79-82.
20. Sigismund PE, Bozzato A, Schumann M, Koch M, Iro H, Zenk J. Management of ranula: 9 yearsŌĆÖ clinical experience in pediatric and adult patients. J Oral Maxillofac Surg 2013;71(3):538-44.
21. Crysdale WS, Mendelsohn JD, Conley S. Ranulas--mucoceles of the oral cavity: Experience in 26 children. Laryngoscope 1988;98(3):296-8.
22. Yang Y, Hong K. Surgical results of the intraoral approach for plunging ranula. Acta Otolaryngol 2014;134(2):201-5.
23. Ogita S, Tsuto T, Tokiwa K, Takahashi T. Intracystic injection of OK-432: A new sclerosing therapy for cystic hygroma in children. Br J Surg 1987;74(8):690-1.
24. Fukase S, Ohta N, Inamura K, Aoyagi M. Treatment of ranula wth intracystic injection of the streptococcal preparation OK-432. Ann Otol Rhinol Laryngol 2003;112(3):214-20.
|
|
||||||||||||||||||||||||||||||||||||||||||

 |
 |